Varicose Veins Treatments
Veins are the vessels that return blood to the heart once it has circulated through the body (as opposed to arteries, which carry oxygen-rich blood from the heart to the body). They have one-way valves that help keep blood flowing in the proper direction. If these valves stop functioning the way they are supposed to, blood can flow backwards and pool in the vein, causing it to stretch.
Varicose veins are swollen, dark blue or purple blood vessels that you can see and feel beneath the skin. They often look like twisted cords, and usually appear on the calves, inside of the legs and ankles. Varicose veins form when the valves within a vein weaken and allow some blood to flow backward. The vein weakens under the additional strain and balloons outward, raising the skin surface.
Patients with varicose veins may experience symptoms of aching, throbbing, heaviness, itching and skin color changes.
Causes and Risks Factors of Varicose Veins
While varicose veins can affect nearly anyone, they tend to occur more often in patients possessing certain risk factors, including:
- Family history of varicose veins
- Pregnancy
- Hormonal changes
- Older age
Varicose veins occur more commonly in women than in men, and the risk tends to increase with age. Many patients with varicose veins are just bothered by their appearance and therefore seek treatment.
Diagnosing Varicose Veins
Dr. Chideckel can usually diagnose varicose veins after a physical examination of the affected area. Additional testing may also be performed, such as an ultrasound to evaluate the structure and blood flow within the veins.
Treatment of Varicose Veins in NYC
Many people with venous disease seek cosmetic treatment to reduce the appearance of varicose or spider veins on the legs. Treatment will relieve the discomfort associated with the condition such as swelling, fatigue, itching and cramps. Sometimes, however, more significant problems can develop if veins are left untreated. Clogging of the blood in the veins can result in the formation of a clot that blocks blood flow or breaks free and travels to the lungs, causing severe damage and even death.
There are several treatment options available to eliminate or reduce the appearance of veins and relieve any symptoms, and may include self-care methods such as losing weight, keeping the legs elevated and wearing compression stockings.
For veins that do not respond to these remedies, more advanced treatments may be required:
- Sclerotherapy treats varicose veins by injecting a solution into the targeted veins that causes them to gradually disappear. The sclerosing solution used during this procedure irritates the vein lining and turns it into scar tissue that eventually fades away. In most cases, desired results are achieved after two to four treatment sessions.
- Endovenous laser therapy is a minimally invasive procedure that treats varicose veins faster, safer and more effectively than other procedures, as it precisely targets the affected veins with a laser probe under ultrasound guidance. The laser energy delivered to the vein damages the vein walls and shrinks the vessel so that blood can no longer flow through and is diverted to healthy veins.
Preventing Varicose Veins
While there is no surefire way to prevent varicose veins from developing, there are certain life changes that can be made in order to reduce your risk of developing this condition. This may include:
- Exercising regularly
- Maintaining a healthy weight
- Eating a diet high in fiber and low in salt
- Elevating the legs
- Avoiding sitting or standing in one position for too long
Dr. Chideckel of NYC will provide you with more information as to how you can reduce your risk of varicose veins and maintain strong vascular health.
» Contact us for more information on Varicose Veins
Spider Veins Treatment
Spider veins, also known as telangiectasias, are small, thin blood vessels visible beneath the skin. They commonly appear on the face or leg, in a shape similar to a spider or a spider web, in either red or blue. In most cases, spider veins are unsightly, causing no other issues.
Spider veins increase with age and can occur to anyone as a result of hormonal changes and pregnancy.
To diagnose spider veins, Dr. Chideckel will perform a physical examination, during which he will inspect the affected area(s). In some cases, an ultrasound may be performed as well to identify the cause of your condition. If you do indeed have spider veins, minimally invasive treatment options are available; Dr. Chideckel will determine which option is most appropriate for your specific condition. The standard treatments for spider veins are sclerotherapy and perhaps VeinGogh.
» Contact us for more information on Spider Veins
Reticular Veins Treatment
Also known as feeder veins, reticular veins are dilated veins that appear blue or green under the skin, affecting as much as 80% of all adults. These veins often develop as a result of genetic factors, but may also be caused by hormonal imbalances or weak veins. Although they do not often cause any painful symptoms or medical complications, many patients are bothered by the appearance of reticular veins and seek treatment to achieve clear, smooth skin.
Sclerotherapy is most often performed to treat reticular veins, while some cases can be treated with a miniphlebectomy, a less invasive alternative to sclerotherapy. Dr. Chideckel will decide which treatment option is best for you after a thorough evaluation of your condition.
» Contact us for more information on Reticular Veins
Deep Vein Thrombosis (DVT) Treatment
Deep vein thrombosis is a serious condition that occurs when a blood clot, also known as a thrombus, forms in a vein deep within the body. Clots most frequently form in the legs as a result of several different factors that can affect blood circulation, and may involve damage to the inner lining of the vein, slow blood flow or thicker blood. Deep vein thrombosis may or may not cause symptoms, but can lead to pulmonary embolism if the clot breaks loose and travels to the lungs.
Blood clots often develop after long periods of inactivity, such as traveling in a car or airplane or prolonged bed rest. They can also be a result of vein damage from injury or surgery, increased pressure from pregnancy or obesity, or a reaction to certain medications. Patients with a family history of DVT and those with heart conditions may be at an increased risk of developing this condition as well. DVT tends to occur most often in patients over the age of 60, although it can occur at any age.
Treatment for deep vein thrombosis aims to keep the blood clot from getting bigger, breaking loose, and causing a pulmonary embolism, as well as reducing the risk of developing another blood clot. This can be accomplished through anticoagulant (blood thinning) medications, thrombolytics to break up the clot or filters to prevent it from traveling to the lungs. Compression stockings can help increase circulation and may be useful in both treating and preventing deep vein thrombosis.
Dr. Chideckel will determine which type of treatment is best for you after a thorough evaluation of your individual condition.
» Contact us for more information on Deep Vein Thrombosis (DVT)
Venous Insufficiency Treatment
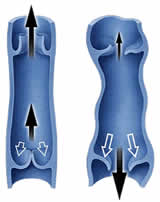 Venous Insufficiency Treatment Manhattan | New York City (NYC)Venous insufficiency is a chronic condition in which blood flows backwards through the leg veins as the result of a failed valve. Instead of returning to the heart, this blood builds up in the leg. If left untreated, venous insufficiency can cause painful symptoms and serious complications.
Venous Insufficiency Treatment Manhattan | New York City (NYC)Venous insufficiency is a chronic condition in which blood flows backwards through the leg veins as the result of a failed valve. Instead of returning to the heart, this blood builds up in the leg. If left untreated, venous insufficiency can cause painful symptoms and serious complications.
Symptoms of venous insufficiency typically include swollen ankles and tightness in the calves at its onset. As the blood builds up, patients may notice that their legs feel tired, heavy or restless. Since venous insufficiency can lead to varicose veins and other uncomfortable conditions, it is important that individuals with the aforementioned symptoms seek medical attention to receive the treatment they need.
Treatment for venous insufficiency varies, depending on the severity of the condition. Mild cases can often be managed by wearing compression stockings, which squeeze the veins and prevent excess blood from flowing backwards; some patients may need to wear compression stockings for the rest of their lives to manage their condition. Other, more severe cases of venous insufficiency may require advanced procedures such as sclerotherapy, ablation and vein stripping. By cutting off blood flow from damaged veins and redirecting it to healthier veins, these procedures ensure that blood can properly flow back to the heart. Only a qualified medical professional can determine which form of treatment is suitable for an individual after a full review of their medical history.
» Contact us for more information on Venous Insufficiency
Venous Skin Ulcer Treatment
Aside from causing complications with blood flow, conditions of the vascular system can also affect the skin and other systems of the body. Also known as a stasis leg ulcer, a venous skin ulcer is a small wound that appears on the skin when the leg veins do not carry blood back to the heart, a condition known as venous insufficiency. Venous skin ulcers develop on the lower leg as a complication of long-term untreated venous insufficiency, and can cause pain, odor, pus, tenderness and redness. Treating venous skin ulcers is usually effective, but this condition can often be prevented by treating venous insufficiency as soon as it occurs.
Patients with untreated venous insufficiency have a high risk of ulcers forming in areas where blood is building up. Pregnant women, as well as those who suffer from deep vein thrombosis and/or obesity, have an increased risk of developing ulcers. Patients can help reduce their risk of developing ulcers by avoiding smoking and alcohol, exercising regularly, eating a balanced diet and taking frequent breaks from standing for long periods of time.
It is important to treat venous skin ulcers as soon as they appear to help facilitate the healing process and prevent infection. Most venous skin ulcers can be treated by improving circulation in the affected area. This can be done by elevating your legs above the level of your heart and by wearing compression stockings to prevent blood from building up in the legs. Skin grafting or vein surgery may be needed to treat ulcers that do not heal within six months or that become infected. Dr. Chideckel will decide which treatment option is best for you.


